Built specifically for independent dental offices
Everything you need to streamline insurance verification and focus on patient care
How it Works
Simple, automated, and seamless integration with your existing workflow
Connects to your PMS and patient calendar
Connects to your PMS and appointment calendar and runs verifications in the background or on demand in minutes.
Automatically verifies eligibility and benefits
Verifies eligibility two weeks in advance and gathers code-level coverage benefits from payer portals and clearinghouses.
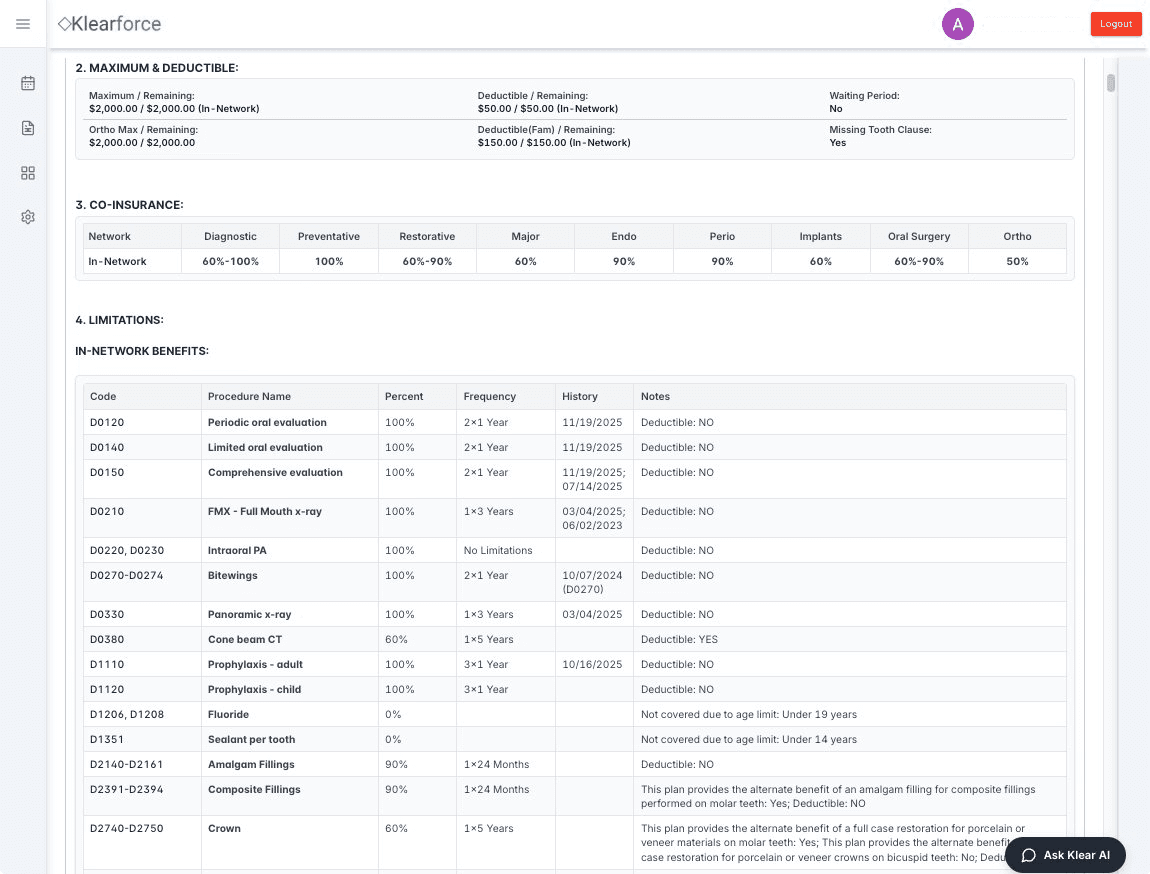
Generates detailed and accurate breakdown summaries
Generates a detailed breakdown summary with ADA code-level benefits, including limitations and history.
Schedule a demo with our team
Learn more about faster, accurate insurance breakdowns
✓
See how Klearforce works with real breakdowns✓
Understand priority support, pricing, and onboarding✓
Get all your questions answered